Substance Use Disorder & Treatment: What is the role of gut health in development and treatment?
 Substance use disorder is a rising problem throughout the world. It has especially become a problem since the beginning of the pandemic. Physicians and therapists are looking for ways to help prevent and stop this disorder from affecting so many people.
Substance use disorder is a rising problem throughout the world. It has especially become a problem since the beginning of the pandemic. Physicians and therapists are looking for ways to help prevent and stop this disorder from affecting so many people.
So let’s take a look at:
- What a substance use disorder is
- What contributes to a substance use disorder
- What is the role of gut health in addiction/substance use disorder
- How to get and stay healthy
What is a Substance Use Disorder?
Substance use disorder is a newer diagnosis. It combines two previous diagnoses: substance addiction and substance dependence. There is now a spectrum, the same way that autism has become a spectrum disorder. This helps physicians and psychiatrists to better diagnose and assist their patients with recovery.
The substance use disorder (SUD) definition is, “a condition in which there is the uncontrolled use of a substance despite harmful consequence.”
For a SUD to be diagnosed, it must consist of 2 or more of the following criteria from the DSM-5.
- “Using in larger amounts or for longer than intended to
- Wanting to cut down/stop using, but not managing to
- Spending a lot of time to get/use/recover from use
- Craving
- Inability to manage commitments due to use
- Continuing to use, even when it causes problems in relationships
- Giving up important activities because of use
- Continuing to use, even when it puts you in danger
- Continuing to use, even when physical or psychological problems may be made worse by use
- Increasing tolerance
- Withdrawal symptoms”
The severity scale progresses through mild (2-3 symptoms), moderate (4-5 symptoms), and severe (6+ symptoms).
There are many different substances that can be abused, but some of the most common are alcohol, nicotine, and medications (prescription and/or over-the-counter).
How do substance use disorders develop?
The development of a SUD is different from person to person. Each case is quite unique and will have different factors in the beginning and continuing development of the disease.
Exposure to a stimulant would be the first part of development. However, it isn’t just using the substance, or frequency of use that causes addiction. Other factors like:
- Age at exposure
- Coexisting mental disorders
- Family history of substance abuse
- Stress/unhealthy ways of dealing with stress
- Emotional distress
- The type of drug itself
- Lifestyle/environment
 Among these, recent studies are suggesting that antibiotic use can have a large factor in SUD development and severity. One study, in particular, shed a lot of light on how much antibiotics can promote chemical brain changes that promote addiction.
Among these, recent studies are suggesting that antibiotic use can have a large factor in SUD development and severity. One study, in particular, shed a lot of light on how much antibiotics can promote chemical brain changes that promote addiction.
In this study, two groups of opioid-dependent mice were given the same opioids and then sent into withdrawal. One group had taken antibiotics so that 80% of their gut microbiomes were depleted, the other took no antibiotics. Both groups of mice seemed to respond the same way to opioid use and withdrawal. That is until they did brain scans.
Brain scans revealed that neuronal recruitment was different between the control groups. The mice who had taken antibiotics had more active neurons in the stress and pain regulating area. This change allows for behavioral changes that would result in a higher tolerance to opioids needed to result in any pain-reducing effects.
This study is important to help doctors to not prescribe medications that can result in opioid misuse when a patient needs antibiotics. This also shows them to be careful with what they prescribe to patients who are already at a heightened risk for SUD.
What is the role of gut health in addiction/substance use disorder?
If we look at the study above, we see that the use of antibiotics was what instigated the changes in the brain’s reactions to opioid use. Whenever antibiotics are used in studies it’s typically to see the difference in a healthy vs unhealthy microbiome.
When there is a healthy balance of microbes, we generally see very healthy people. When someone is experiencing dysbiosis of any sort, we will see them presenting with different types of malaise. The unhealthy microbes within our gut can send chemicals and other signaling molecules all throughout our bodies to cause inflammation and other problems that lead to disease.
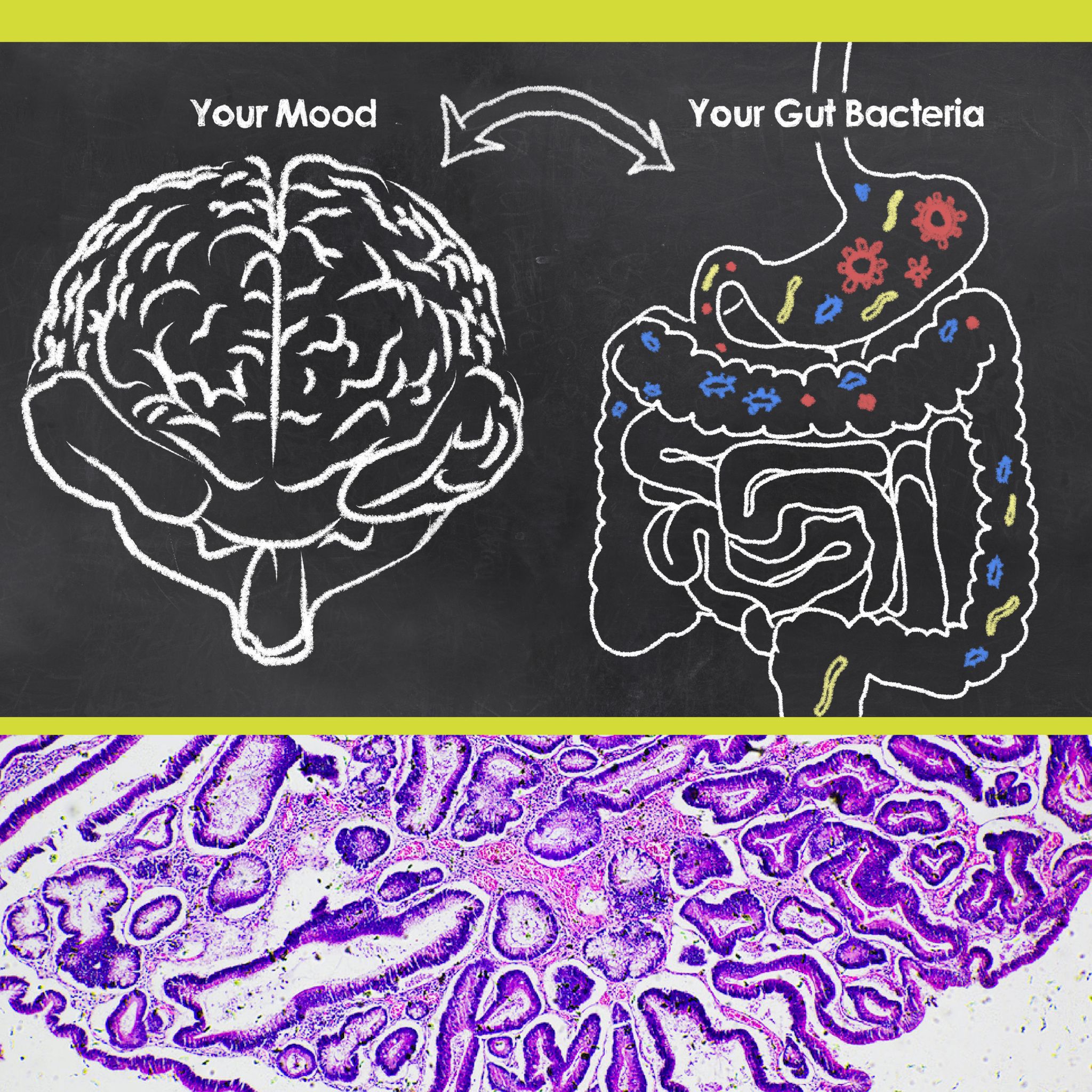
When these molecules affect our brain it can change our mood, behavior, and pretty much everything else. This is where addictions can happen.
Once the chemical changes happen, our brains are rewired to crave more of the substances and we become addicted or dependent on them.
Sometimes the drugs themselves can alter our microbiome and cause dysbiosis. So let’s take a look at a few of the common addictions people have and how they specifically work with the gut microbiome. (our example for opioids can be seen above)
Alcohol
Alcohol is one of the most abused substances on the market. You’ve probably experienced an upset stomach after drinking, so it isn’t much of a surprise that your gut is affected by alcohol. (we have a whole article on this already)
The effects of alcohol abuse and the gut microbiome are known to affect sociability and increase depression rates. This is linked to the decrease in β-hydroxybutyrate (BHB) synthesis. The ethanol in alcohol affects the liver’s ability to synthesize BHB. When tested in a human to mice microbiota transplantation the mice showed similar results — equating it to a gut microbiome-related complication.
This results in lower amounts of BHB found in the brain and leads to depression, social impairments, and brain alterations. All of this can lead to an endless cycle that promotes alcohol abuse.
Nicotine
Nicotine is the main addictive substance found in tobacco and cigarettes. Nicotine has been linked to:
- Increased intestinal permeability (leaky gut)
- Lower microbial diversity
- Less healthy and more unhealthy bacteria residing in the microbiome
- Undesirable alterations to the entire digestive tract
All of these promote systemic inflammation and the circulation of unhealthy molecules. This can lead to cancer and other diseases as a result. These changes often affect the liver, lungs, and brain chemistry.
When patients stop smoking, they were found to have improved every one of the issues mentioned above.
Nicotine also seems to affect men and women differently which can explain why each gender has different obstacles to overcome when trying to quit.
How to Keep Your Gut and Mind Healthy
 Since the gut has so much effect on how your body responds to stimuli, we thought we would share some of the best ways to keep your gut balanced to avoid any unnecessary negative problems in the future.
Since the gut has so much effect on how your body responds to stimuli, we thought we would share some of the best ways to keep your gut balanced to avoid any unnecessary negative problems in the future.
- Eat a variety of healthy foods daily
- Avoid eating unhealthy foods
- Avoid substance use (especially if you feel like you are stressed and might go overboard)
- Learn to relax — find a hobby that lets you relax like reading or writing. Or try meditating, take a bath, or getting a massage.
- Exercise regularly (this can be a way to relax) — going for a walk, doing yoga, taking martial arts, etc.
- Take yourself out of stressful situations
- Try to get into a healthier sleeping routine
- Take Atrantil or other prebiotic/postbiotics to help support good gut health
Substance use disorder can be a scary thing for the person experiencing it and those around them. If you or a loved one are struggling, talk to a doctor immediately to get help. Ask your doctor or medical professional if adding any of these suggestions to your daily routine can help your individual case. There are so many resources to help improve this condition, and it just takes one step to start and a few to keep going.
SAMHSA’s National Helpline at 1-800-662-HELP (4357)
- https://www.psychiatry.org/patients-families/addiction
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5525418/
- https://www.eneuro.org/content/7/3/ENEURO.0312-19.2020
- https://www.cell.com/cell-reports/fulltext/S2211-1247(20)31227-4?_returnURL=https%3A%2F%2Flinkinghub.elsevier.com%2Fretrieve%2Fpii%2FS2211124720312274%3Fshowall%3Dtrue#secsectitle0075
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8218903/#s4title
- https://pubmed.ncbi.nlm.nih.gov/29035044/